You deserve clear, simple answers when a painful tooth problem threatens your smile. This guide explains what a modern root canal treatment is and how it helps remove infected pulp, disinfect the interior spaces, and seal the area to prevent reinfection.
Most procedures finish in one or two visits with local anesthesia, so the experience is often similar to a routine filling. After the appointment, numbness may last a few hours, and you should avoid chewing until it wears off.
Saving your natural tooth preserves chewing function, maintains your bite, and can cost less than extracting and replacing the tooth with an implant or bridge. Your dentist—or an endodontist for complex cases—cleans, shapes, and seals the canal spaces to protect long-term oral health.
Key Takeaways
- Modern care focuses on saving your natural tooth and restoring comfort.
- The process cleans infected pulp, seals spaces, and prevents reinfection.
- Most people find the procedure no more uncomfortable than a standard dental procedure.
- Expect one or two visits; time varies with tooth complexity.
- Keeping a tooth preserves bite, appearance, and overall oral health.
- An endodontist may help when anatomy is complex.
What Is Root Canal Treatment and Why You Might Need It
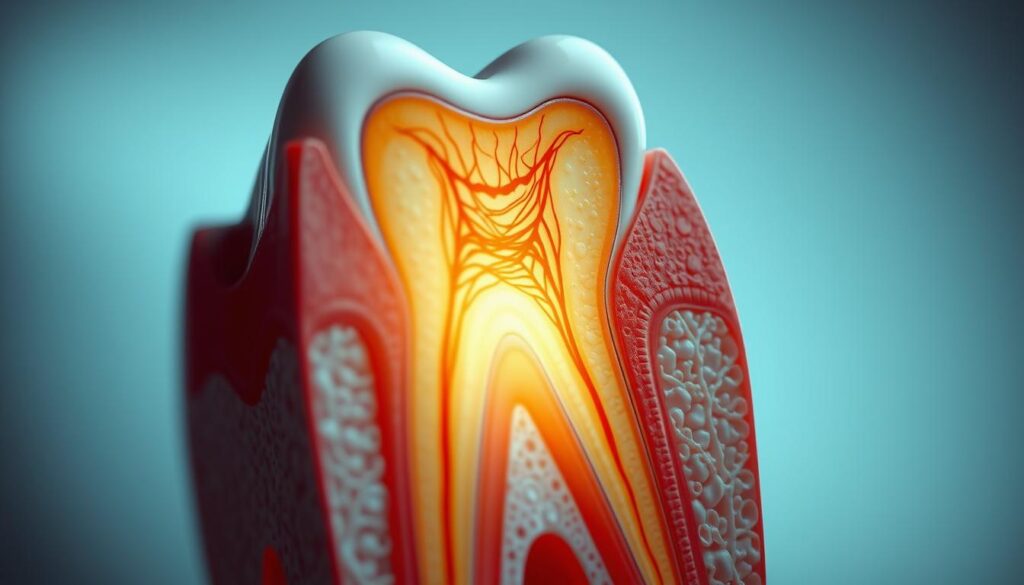
Inside the tooth: beneath enamel and dentin lies the pulp — a soft tissue with nerves, blood vessels, and connective tissue that helps the tooth develop.
You can still use a mature tooth even after the pulp is removed because surrounding tissues keep it nourished. However, the pulp can become inflamed or infected from deep decay, repeated dental work, faulty crowns, cracks, chips, or trauma.
If bacteria reach this inner tissue, infection may spread through the root tip into nearby bone. That can cause an abscess, swelling, and persistent pain if you leave it untreated.
When you might need this procedure
- Deep cavities or a visible crack that exposes the pulp.
- Lingering sensitivity, severe pain when biting, or swelling near the tooth.
- Repeated procedures or a damaged crown that lets bacteria enter the canal spaces.
Your dentist will evaluate the tooth anatomy and decide if saving the tooth with canal therapy is possible. In complex anatomy, a specialist may be recommended.
To learn more about options and steps, read about canal treatment.
Signs You May Need a Root Canal
Watch for persistent tooth sensitivity to hot or cold that lingers after the sip or bite. This lasting reaction is one of the clearest symptoms that the pulp or inner spaces may be affected.

Lingering sensitivity to hot or cold
If heat or chill keeps causing sharp pain after the source is gone, schedule an exam. Your dentist will test the area and may take X‑rays to see if the inner tissue is inflamed or infected.
Severe pain when chewing or biting
Throbbing or sharp pain on biting often means the nerve or surrounding area is irritated. If the pain wakes you at night or worsens with pressure, you may need root canal care quickly.
Swollen or tender gums, pimples on the gums
Swelling, tenderness, or a pimple‑like bump can indicate drainage from an infection near the root tip. Do not ignore these signs — infections do not heal on their own.
- Deep decay, a chipped or cracked tooth, or darkened gums can let bacteria enter the inner spaces.
- Sensitivity without visible decay still warrants testing by a dentist.
- If symptoms persist or the anatomy is complex, ask for a referral to an endodontist.
If you think you need root canal urgently because of severe pain or swelling, avoid chewing on that side and call your clinic. For more on options and canal treatment, see canal treatment options.
Root Canal Treatment Procedure: Step-by-Step
Your dentist begins by numbing the area and isolating the tooth to keep the field clean and comfortable.
Anesthesia and isolation: Local anesthesia makes the visit comfortable. A dental dam keeps saliva and bacteria away so the dentist can work in a dry field.
An access opening and pulp removal
The dentist makes a small opening in the tooth to reach and remove the inflamed or infected pulp. Removing that tissue relieves pressure and pain.
Cleaning, shaping, and irrigation
Special files clean and shape the canals inside the root. Antimicrobial solutions flush out debris and reduce infection risk.
Filling, sealing, and final restoration
After drying, the canals are filled with a rubber-like material called gutta-percha and sealed with adhesive cement. A temporary filling closes the access.
You will usually return for a crown or a permanent filling to restore strength and function. Most cases finish in one or two appointments, with sessions from about 90 minutes to several hours depending on complexity. Expect numbness for 2–4 hours after the visit; avoid chewing until sensation returns.
Benefits, Comfort, and Safety of Root Canal Therapy
B
Saving a damaged tooth helps you chew efficiently and keeps neighboring teeth from shifting. This choice preserves bite force, looks natural, and often costs less than replacing the tooth.
Saving your natural tooth and restoring function
You keep your original tooth, which supports chewing and jaw stability. A well‑fitted crown or durable filling restores strength and lowers the chance of future cracks.
Is a root canal painful? What to expect with anesthesia
With local anesthesia, most people find the procedure as comfortable as a routine filling. You may have short‑term soreness or numbness that eases in a few days.
Potential risks and how dentists prevent reinfection
Reinfection can occur if canals are missed or the seal fails. Your dentist or an endodontist reduces risk with careful cleaning, disinfection, and a reliable final restoration.
| Benefit | Why it matters | What your dentist does |
|---|---|---|
| Keep natural tooth | Maintains chewing, look, and bone | Restore with crown or filling |
| Comfort during visit | Minimal pain with anesthesia | Local anesthesia and breaks |
| Lower reinfection risk | Long‑term success when sealed | Thorough cleaning and sealing |
Recovery and Aftercare: What Happens After a Root Canal
The hours and days after the procedure set the stage for a smooth recovery and fewer complications. Follow simple steps at home to reduce pain and protect the temporary material until your final restoration is placed.
The first 24-48 hours: numbness, soreness, and swelling
Expect numbness for about 2–4 hours. Mild soreness or slight swelling may appear for a few days as the area heals.
If swelling is noticeable, apply a cold pack in short intervals and rest. Most people return to work or school the same day unless they had sedation.
Eating and chewing: when to avoid hard or sticky foods
Avoid chewing on the treated tooth until numbness fully wears off. If you have a temporary filling or crown, stick to soft foods and skip hard or sticky items that could dislodge the material.
Pain relief, antibiotics, and medications
Over-the-counter medication like ibuprofen or acetaminophen manages most discomfort. Take antibiotics only if your dentist prescribes them for signs of infection.
Red flags: severe pain, swelling, or fever
Call your dentist right away if pain worsens, swelling increases, or you develop a fever. These can be signs of a persistent infection that needs prompt attention.
- Short-term care: Brush gently and maintain normal hygiene near the area.
- Plan your time: Rest if needed; the first 48 days are most sensitive.
- Follow-up: Schedule the final crown or permanent filling to seal out infection and restore full function.
Costs and Alternatives in India: What to Consider
Your final bill depends on anatomy, chosen materials, and whether a specialist performs the care.
What affects price: tooth type, complexity, and materials
Molars usually cost more because they often have multiple canals and complex roots. Curved roots, prior procedures, or active infection can add visits and fees.
Material choices for the final crown or filling change the total. A high‑quality crown protects the tooth and often saves money long term.
Insurance, clinics, and dental schools
Fees vary across private clinics, hospital dental departments, and dental colleges. Student clinics offer lower rates under supervision.
Check insurer limits, covered dental procedures, and waiting periods before you commit.
Extraction versus saving the tooth
Removing a tooth then replacing it with an implant or bridge usually costs more overall than preserving it with root canal treatment plus a crown.
If anatomy is complex, an endodontist-led approach may cost more up front but can avoid repeat work later.
| Factor | How it raises cost | What to ask your dentist | Typical impact |
|---|---|---|---|
| Tooth type | Molars need more chair time and instruments | How many canals and expected visits? | Moderate–High |
| Materials | Premium crowns and core build-ups increase fees | Compare cement, crown type, and warranty | Moderate |
| Provider | Specialist care or private clinic may charge more | Is an endodontist recommended for my tooth? | Low–High |
| Alternatives | Extraction + implant/bridge adds surgery and lab costs | Full cost estimate and timeline for replacement? | High |
Tip: Ask for a written plan that lists procedures, visits, materials, and warranties. Completing the final crown promptly protects your oral health and reduces future spending.
Conclusion
If you act quickly, saving a damaged tooth is often safer and less costly than replacing it later. Consult your dentist, and ask about options if you notice lingering sensitivity, swelling, or a gum pimple.
Root canal therapy removes infected pulp from inside the tooth, cleans and seals the canals, and restores the area with a filling or crown. Most people complete this dental procedure in one or two visits with local anesthesia and return to normal life quickly.
Choosing timely canal treatment may also avoid more complex work after a chip, deep cavity, or ongoing pain. If you think you need root canal, book an exam and get a clear plan for restoration and aftercare.